Private PrEP Co-pay Assistance Programs for Underinsured Patients
- Provider Referral Form for Kaiser Clients Only Pre-Exposure Prophylaxis Assistance Program (PrEP-AP) The client below is newly enrolled in the PrEP-AP administered by the California Department of Public. Please do not charge the client a copay for PrEP-related services for any reason.
- Kaiser Permanente Insurance Company provides certain administrative services for the Plan and is not an insurer of the Plan or financially liable for health care benefits under the Plan. Kaiser Foundation Health Plan, Inc., in Northern and Southern California and Hawaii. Kaiser Foundation Health Plan of Colorado. Kaiser Foundation Health.
- Financial Assistance for HIV & PrEP HIV and PrEP medications can be expensive, and for those struggling financially, copay assistance programs may help bridge the gap. Kaiser Permanente coordinates with several manufacturers and foundations to help patients who are eligible and qualify. There is no guarantee of availability.
- This site can help you enroll in the co-pay program and activate or replace your co-pay coupon card. If you would like to speak to someone directly, please call 1-877-505-6986 1-877-505-6986. When enrolling you will have to answer a few questions to confirm you are eligible for the program. This program covers a set amount in co-pays per year.
Kaiser Permanente Washington Specialty Pharmacy: HIV & PrEP services. The objective of the Specialty Pharmacy’s HIV (human immunodeficiency virus) and PrEP (pre-exposure prophylaxis) services is to help you get maximum benefit from your medications and treatment plan.
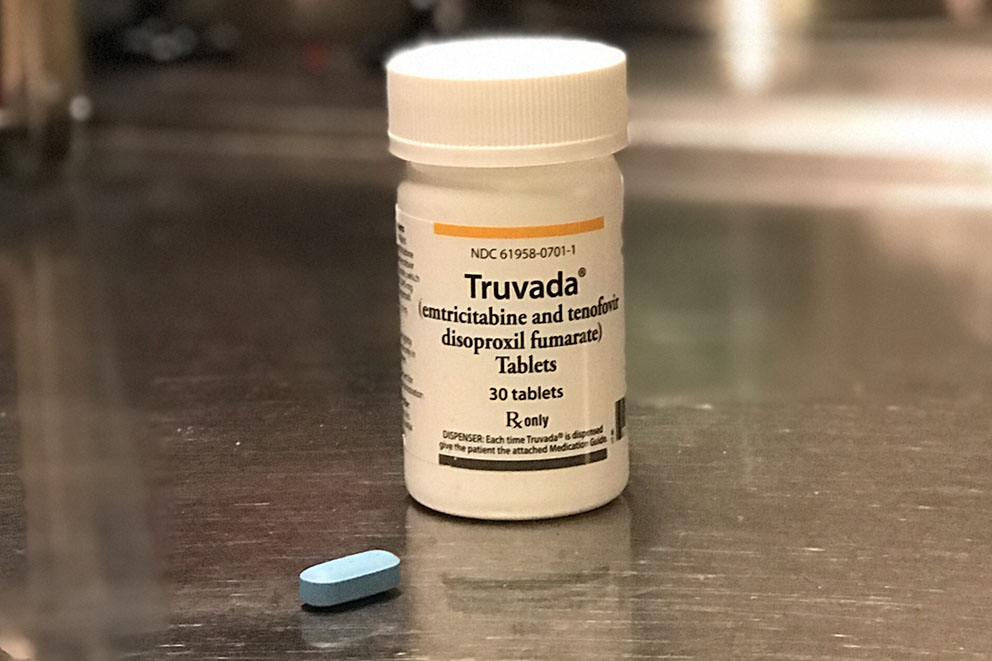
Gilead Advancing Access is a co-pay assistance program available from the manufacturer of Truvada and Descovy, the two medications approved for PrEP.
WHAT IT COVERS: The co-pay card covers the patient’s out-of-pocket costs for either of the two medications up to $7,200 per year. It does not cover out-of-pocket costs for clinical visits or labs.
WHO IS ELIGIBLE: It is available to individuals who have private health plan coverage, including Marketplace plans like the ones on PrEPcost.org, and to those with employer-sponsored plans. There are no income restrictions to access this program.
HOW IT WORKS: Follow the link below or call 1-877-505-6986 for assistance. Complete the online application, selecting Co-pay Support, then “Truvada” or 'Descovy' for the medication, and indicate that you intend to use it “to reduce the risk of getting HIV-1.” You will know immediately if you are eligible for assistance. Save or print the program’s card to use to pay for the medication at the pharmacy.
ENROLLMENT LINK: https://www.gileadadvancingaccess.com/
NOTE: Kaiser Permanente health plans require clients to apply for the Gilead Co-pay Coupon Card, then pay for the medication directly and submit a reimbursement form through the website: www.patientrebateonline.com
The Patient Advocate Foundation offers a Co-Pay Relief Program that is available for PrEP.
WHAT IT COVERS: It covers the patient’s out-of-pocket costs for the medication up to $7,500 per year. It does not cover out-of-pocket costs for clinical visits or labs.
WHO IS ELIGIBLE: It is available to individuals who have health insurance that covers Truvada® and whose income falls below 400% of the Federal Poverty Guideline, adjusted by the Cost of Living Index and the number in the household.
HOW IT WORKS: Follow the link below, or call 1-866-512-3861, Option 1 for assistance. Register for the program and then complete the online application. You will know if you are eligible for assistance within 10 minutes of submitting the application. An income verification may also be required.
In addition to the programs outlined above, other financial assistance may be available based on health insurance type and income. Good Days offers co-pay assistance for PrEP for individuals with Medicare or Military insurance coverage. Co-pay assistance from the PAN Foundation may also be available for PrEP patients with Medicare coverage, although this program is currently closed.
A number of states have established their own PrEP Assistance Programs. Most cover out-of-pocket expenses for the medication as well as clinical visits and labs, see the table below.
In most of these states, both the PrEP patient and the provider must complete an application to participate in the program. Please follow the link to your state’s program for more information.
*In these states, PrEP medication assistance is only available through local health department clinics or select contracted providers.
Some PrEP Assistance Programs may consider providing medication assistance to PrEP candidates on a case by case basis when the individual is categorically ineligible for health insurance coverage or cannot use their health insurance plan for PrEP.
California: For questions about the PrEP-related medical out-of-pocket benefit, please call (877) 495-0990. For more information about benefits and enrollment, please visit: www.cdph.ca.gov/Programs/CID/DOA/Pages/OA_adap_benefits_prepAP.aspx.
Colorado: For more information about the program or to enroll online, visit www.coenroll.com. Visit www.proudtobeprepped.com to learn about the different options to pay for PrEP in Colorado.
District of Columbia: For more information visit: https://dchealth.dc.gov/node/1333931 or call the program at: (202) 671-4815.
Florida: Call 1-850-245-4422 for more information about Florida’s PrEP Drug Assistance program and participating health department clinics.
Softether vpn client for mac download. Illinois: For more information about the program or to enroll online, visit www.prep4illinois.com, or call the program’s hotline: 1-800-825-3518.
Massachusetts: Visit the program’s website to find out more: https://crine.org/hdap/prep-drug-assistance-program/ or call CRI’s PrEP Coordinator at 617-502-1737 (or toll free at 800-228-2714 x3737).
New York: Call 1-800-542-2437 to enroll and for more information, visit: https://www.health.ny.gov/diseases/aids/general/resources/adap/index.htm.
Ohio: Scheduled to launch at the beginning of 2019. Please visit www.ohiv.org or call the state’s HIV/STD hotline 1-800-332-2437 for more information.
Virginia: Call 1-800-533-4148 for more information about Virginia’s PrEP Drug Assistance Program and participating providers.
Washington State: Please visit www.doh.wa.gov/prepdap or call 1-877-376-9316 for more information.
Private PrEP Medication Assistance Program for Uninsured Patients
For uninsured individuals, the Gilead Advancing Access Medication Assistance Program can help cover the cost of Truvada or Descovy for PrEP.
WHAT IT COVERS: The program provides financial assistance to pay for Truvada or Descovy, the two medications for PrEP. It does not cover the cost of clinical visits or labs.
WHO IS ELIGIBLE: The program is available to uninsured individuals, regardless of immigration status. The household income limit for the program is 500% FPL ($60,300 per year in all states except Hawaii and Alaska). Applicants will be asked to submit further documentation as proof of income.
HOW IT WORKS: Follow the link below or call 1-800-226-2056 for assistance. Complete the online application, selecting “Uninsured Support,” then “Patient Assistance Program (PAP) Eligibility Screening.” Select “Truvada” or 'Descovy' for the medication, indicate that you intend to use it for PrEP, and enter your personal information. Your PrEP provider will also need to complete a portion of the application.
ENROLLMENT LINK: https://www.gileadadvancingaccess.com
About Insuring Your Health
KHN contributing columnist Michelle Andrews writes the series Insuring Your Health, which explores health care coverage and costs.
To contact Michelle with a question or comment, click here.
Since Kristen Catton started taking the drug Gilenya two years ago, she’s had only one minor relapse of her multiple sclerosis, following a bout of the flu.
She can walk comfortably, see clearly and work part time as a nurse case manager at a hospital near her home in Columbus, Ohio. This is a big step forward; two drugs she previously tried failed to control her physical symptoms or prevent repeated flare-ups.
This year, Catton, 48, got a shock. Her health insurance plan changed the way it handles the payments that the drugmaker Novartis makes to help cover her prescription’s cost. Her copayment is roughly $3,800 a month, but Novartis helps reduce that out-of-pocket expense with payments to the health plan. The prescription costs about $90,000 a year.
Those Novartis payments no longer counted toward her family plan’s $8,800 annual pharmacy deductible. That meant once she hit the drugmaker’s payment cap for the copay assistance in April, she would have to pay the entire copayment herself until her pharmacy deductible was met.
Catton is one of a growing number of consumers taking expensive drugs who are discovering they are no longer insulated by copay assistance programs that help cover their costs. Through such programs, consumers typically owe nothing or have modest monthly copayments for pricey drugs because many drug manufacturers pay a patient’s portion of the cost to the health plan, which chips away at the consumer’s deductible and out-of-pocket maximum limits until the health plan starts paying the whole tab.
Since her insurance company changed its rules, Kristen Catton is responsible for nearly $9,000 of the cost of her multiple sclerosis drug.(Courtesy of Kristen Catton)
Under new “copay accumulator” programs, that no longer happens.
In these programs, the monthly copayments drug companies make don’t count toward patients’ plan deductibles or out-of-pocket maximums. Once patients hit the annual limit on a drugmaker’s copay assistance program, they’re on the hook for their entire monthly copayment until they reach their plan deductible and spending limits.
Catton put the $3,800 May copayment on a credit card. She knows her insurer will start paying the entire tab once she hits the pharmacy deductible. But, she said, she can’t afford to pay nearly $9,000 a year out-of-pocket for the foreseeable future.
“I’m talking to my doctor to see if I can I take it every other day,” she said. “I guess I’m winging it until I can figure out what to do.”
Drug copay assistance programs have long been controversial.
Proponents say that in an age of increasingly high deductibles and coinsurance charges, such help is the only way some patients can afford crucial medications.
But opponents say the programs increase drug spending on expensive brand-name drugs by discouraging people from using more cost-effective alternatives.

Email Sign-Up
Switching to a cheaper drug may not be an option, said Bari Talente, executive vice president for advocacy at the National Multiple Sclerosis Society.
“Generally the multiple sclerosis drugs are not substitutable,” she said. “Most have different mechanisms of action, different administration and different side effect profiles.” Generics, when they’re available, are pricey too, typically costing $60,000 or more annually, she said.
Most MS drug annual copay assistance limits, if they have them, are between $9,000 and $12,000, Talente said.
Employers argue that the drug copayment programs are an attempt to circumvent their efforts to manage health care costs. For example, employers may try to discourage the use of a specialty drug when there’s a lower-cost drug available by requiring higher patient cost sharing.
There’s also the issue of fairness.
“From an employer perspective, everyone under the plan has to be treated the same,” said Brian Marcotte, president and CEO of the National Business Group on Health (NBGH), which represents large employers.
If someone needs medical care such as surgery, for example, that person doesn’t get help covering his deductible, while the person with the expensive drug might, he said.
According to an NBGH survey of about 140 multistate employers with at least 5,000 workers, 17 percent reported they have a copay accumulator program in place this year, Marcotte said. Fifty-six percent reported they’re considering them for 2019 or 2020.
If there is no comparable drug available, drug copayment programs may have a role to play if they can be structured so that participating patients are paying some amount toward their deductible, Marcotte said. But, he said, assistance programs for drugs that are available from more than source, such as a brand drug that is also available as a generic, shouldn’t be allowed.
In 2016, 20 percent of prescriptions for brand-name drugs used a drug copay assistance coupon, according to an analysis by researchers at the USC Schaeffer Center for Health Policy and Economics. Among the top 200 drugs based on spending in 2014, the study found that 132 were brand-name drugs, and 90 of them offered copay coupons. Fifty-one percent of the drugs with copay coupons had no substitute at all or only another brand drug as a close therapeutic substitute, the analysis found.
Advocates for people with HIV and AIDS say copay accumulators are cropping up in their patients’ plans and beginning to cause patients trouble. Drugs to treat HIV typically don’t have generic alternatives.

The biggest impact for the community their organizations serve may be for PrEP, a daily pill that helps prevent HIV infection, said Carl Schmid, deputy executive director at the AIDS Institute, an advocacy group. A 30-day supply of PrEP (brand-name Truvada) can cost nearly $2,000. Drug manufacturer Gilead offers a copay assistance program that covers up to $3,600 annually in copay assistance, with no limit on how much is paid per month.

“They’re at risk for HIV, they know it and want to protect themselves,” Schmid said. “It’s a public health issue.”
Earlier this month, the AIDS Institute was among 60 HIV organizations that sent letters to state attorneys general and insurance commissioners across the country asking them to investigate this practice, which has emerged in employer and marketplace plans this year.
Compounding advocates’ concerns is the fact that these coverage changes are frequently not communicated clearly to patients, Schmid said. They are typically buried deep in the plan documents and don’t appear in the user-friendly summary of benefits and coverage that consumers receive from their health plan.
“How is a patient to know?” Schmid asks. They learn of the change only when they get a big bill midway through the year. “And then they’re stuck.”
Kaiser Copay Cost
KHN’s coverage of prescription drug development, costs and pricing is supported in part by the Laura and John Arnold Foundation.
